Nipple and Oral Thrush | The Complete Guide of Treatment Options
Let's tackle thrush today, shall we?
What is thrush?
Thrush is the more memorable, easy-to-say term to describe candidiasis - an overgrowth of one of many yeasts in the Candida family. Most commonly, the culprit is Candida albicans, but other yeast species may be to blame.
Though thrush may describe yeast overgrowth in any location, in the context of human milk feeding, thrush primarily refers to symptoms in one of two areas; an infant's mouth (pseudomembranous candidiasis) or the breast/mammary gland (mammary candidiasis).
What causes thrush?
Candida albicans is no stranger - potentially up to 60% of the population has it somewhere on the body. When an organism is present in or on our bodies but doesn't cause any problems, it's considered commensal, aka friendly.
Usually, Candida albicans and the other Candida species live on us - primarily in the GI tract, including mouth and anus, and in the vagina for vagina having folk- without causing any problems.
Sometimes, however, the yeast can get too homey and grow to such a large number it becomes problematic, aka pathogenic.
Factors that contribute to this switch include
Antibiotic use
Age; Babies and the elderly are more prone to developing thrush
Reduced/compromised immune system
Generally, a baby who develops thrush within the first 4-6 weeks became colonized with the yeast via the birth canal, whether or not the parent had an active vaginal yeast infection.
Because pregnant folks are more prone to vaginal yeast infections than their non-pregnant friends, the likelihood that one will have a vaginal yeast infection at the time of delivery may be higher than you might imagine.
Not all babies born vaginally to a parent with an active vaginal yeast infection will develop thrush. And thrush can develop due to other mechanisms of exposure, which is why babies born via C-section can also be colonized with Candida albicans and/or develop thrush.
What are the signs & symptoms of thrush?
While the signs/ symptoms of thrush are not hard to identify, it may be hard to know for sure if what you're seeing is actually thrush vs. something else.
And as you will come to read, the well-known symptoms we once attributed to thrush of the breast may not even be related to yeast at all!
I find that identifying thrush in babies is the easiest as it's more objective.
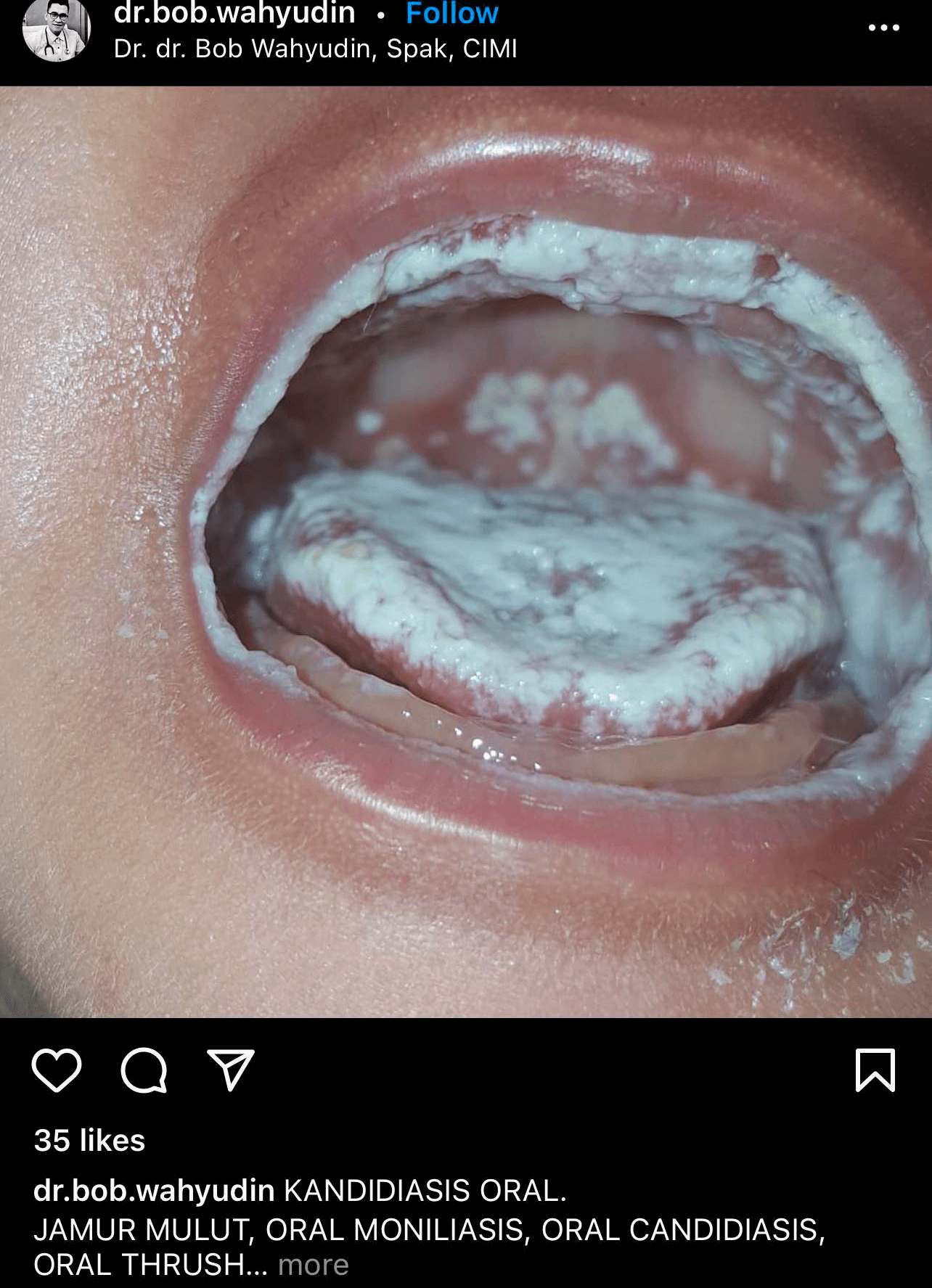
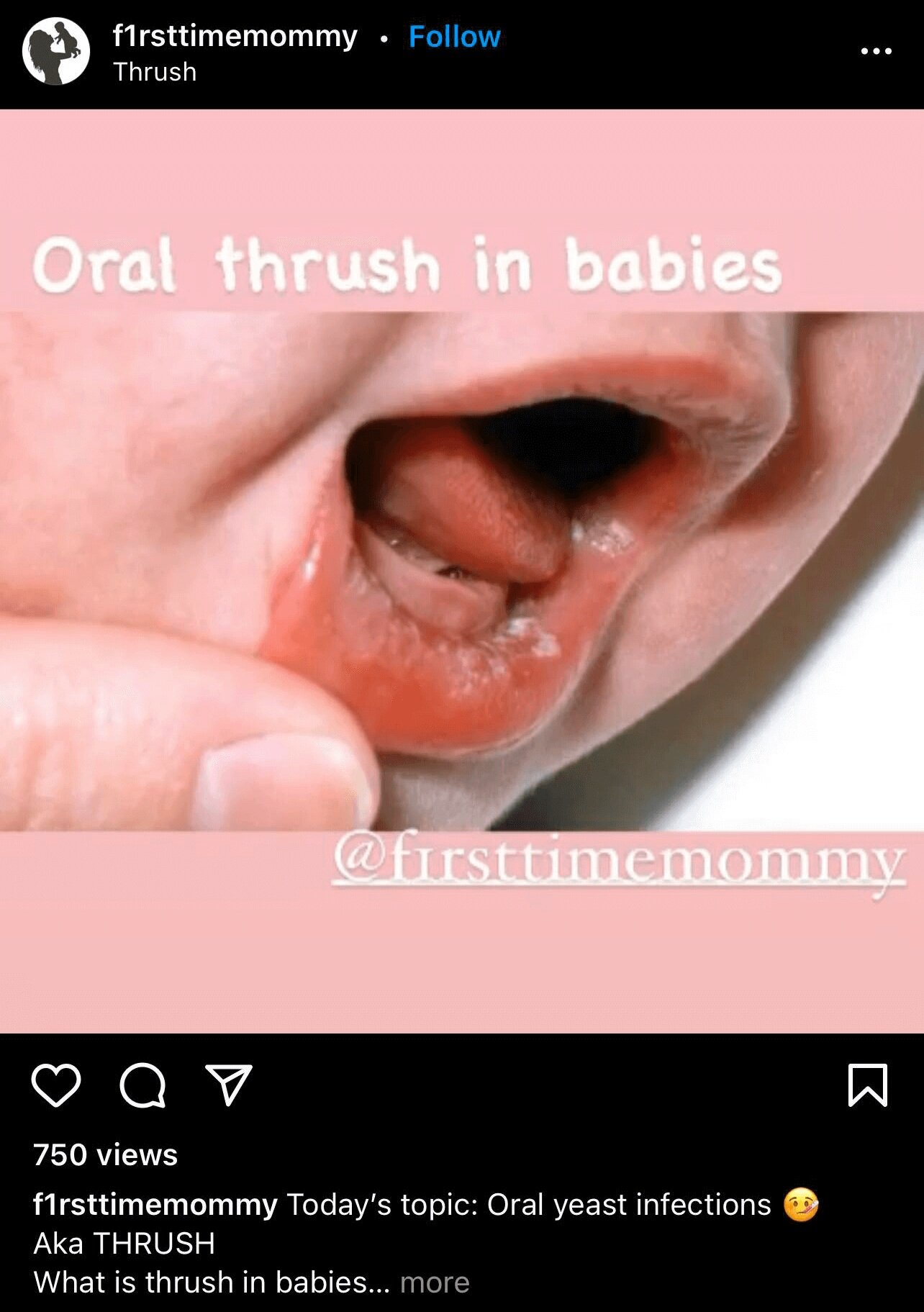
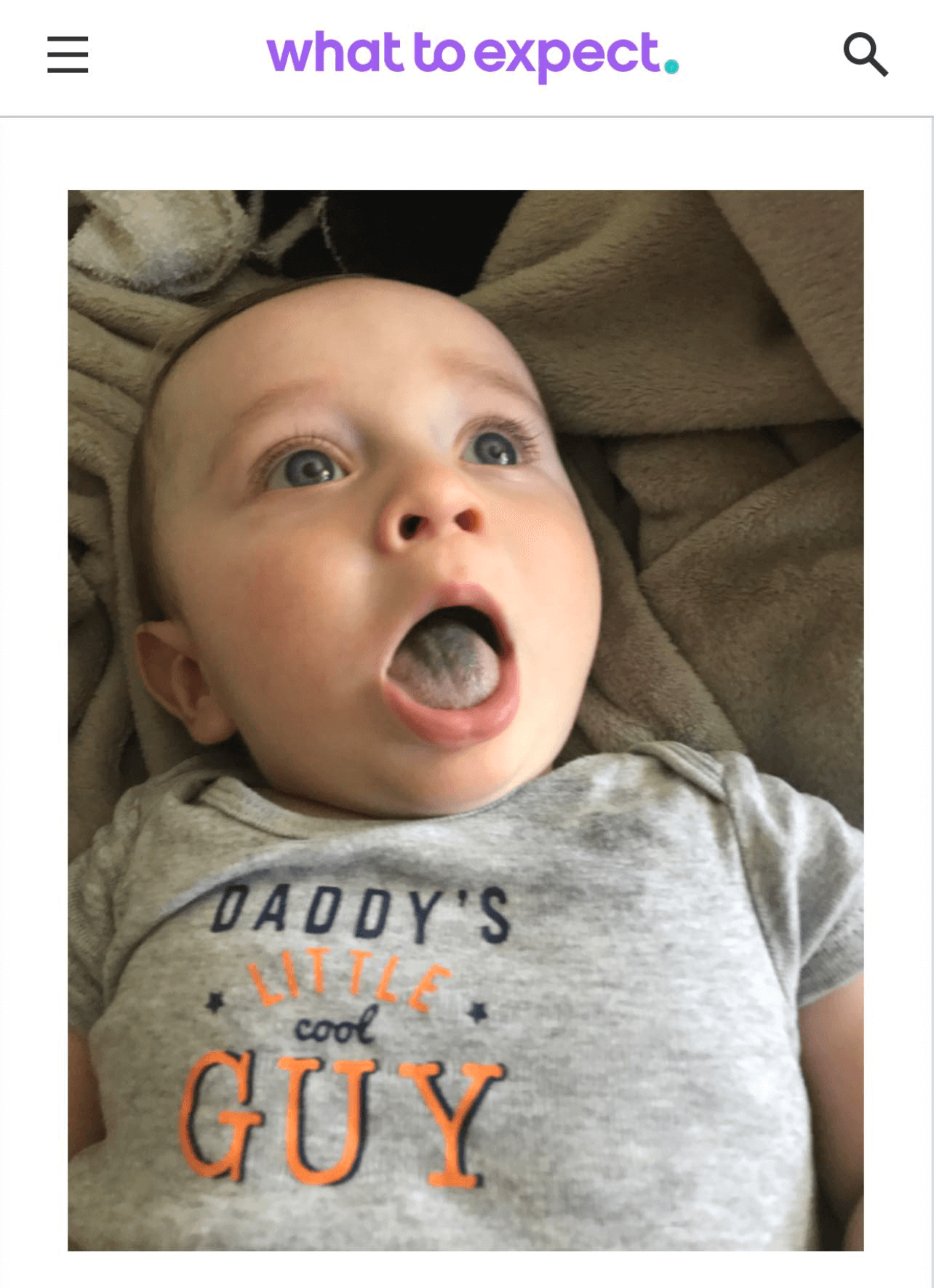
Thrush in babies
Oral thrush (pseudomembranous candidiasis) is characterized by white-yellow, cottony patches on the lips, cheeks, and/or tongue.
These patches may look like "curds" or a very thick white film, which are easy to wipe off. Under these patches, the skin (mucosa) underneath may look a bit angry- red & irritated.
Generally, thrush does not ONLY cover the tongue, and even more rarely will it be limited to JUST the top surface of the tongue.
Oral thrush may cause discomfort, which can lead to feeding challenges. Frequent popping on and off and feeding refusal is not uncommon in babies who have bothersome cases of thrush.
For many babies, though, it doesn't bother them at all.
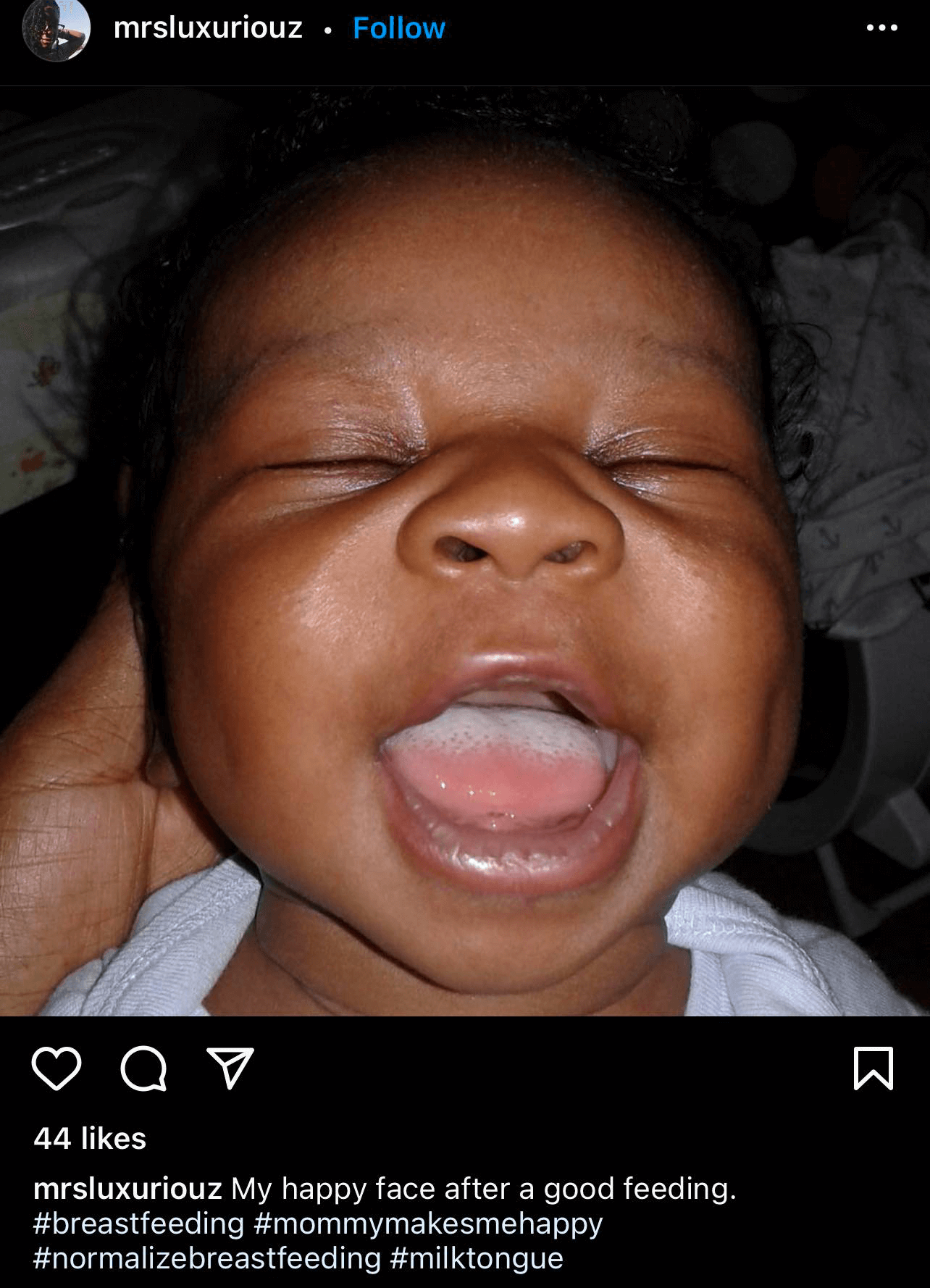
Thrush vs. Milk Tongue
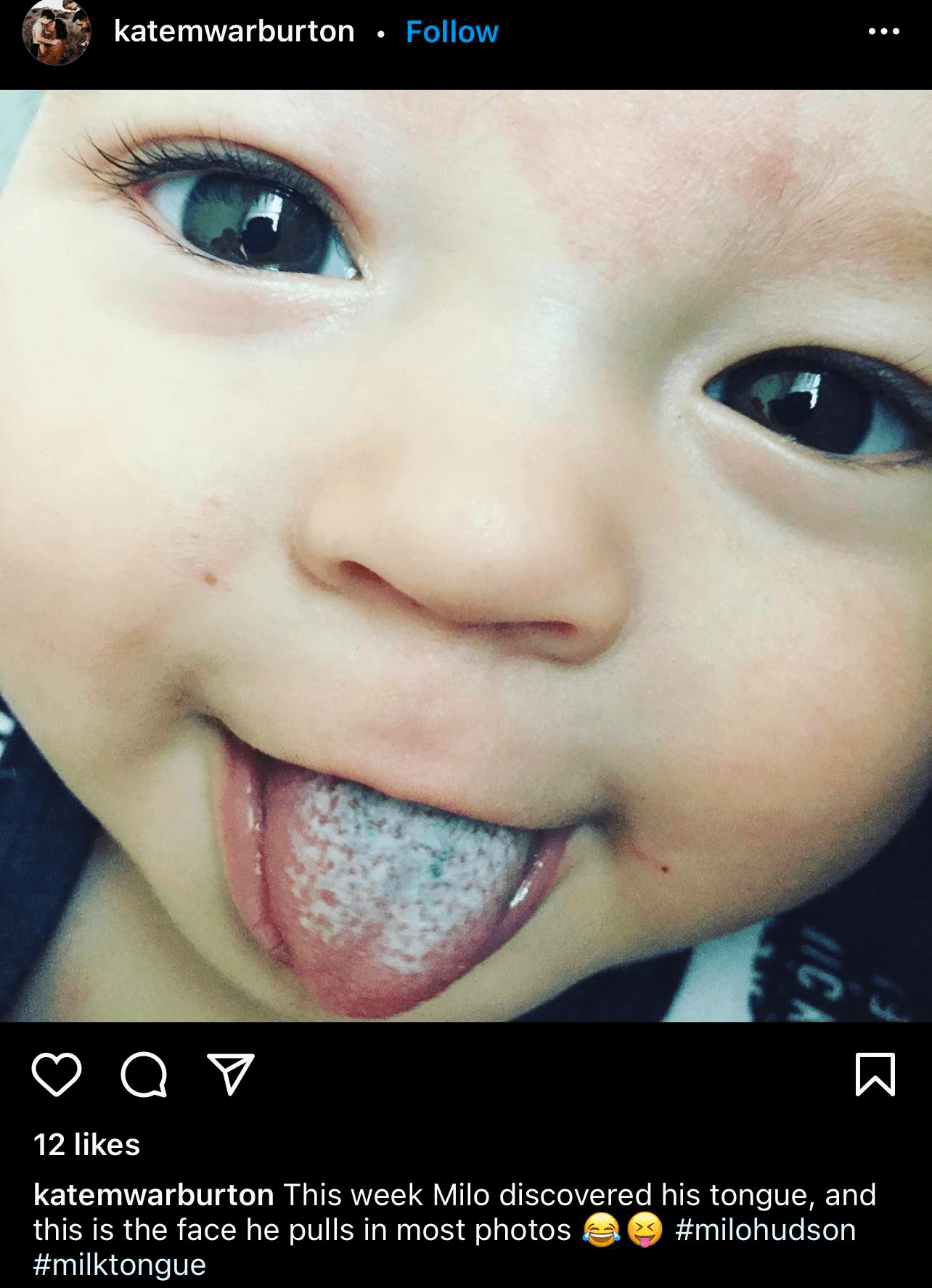
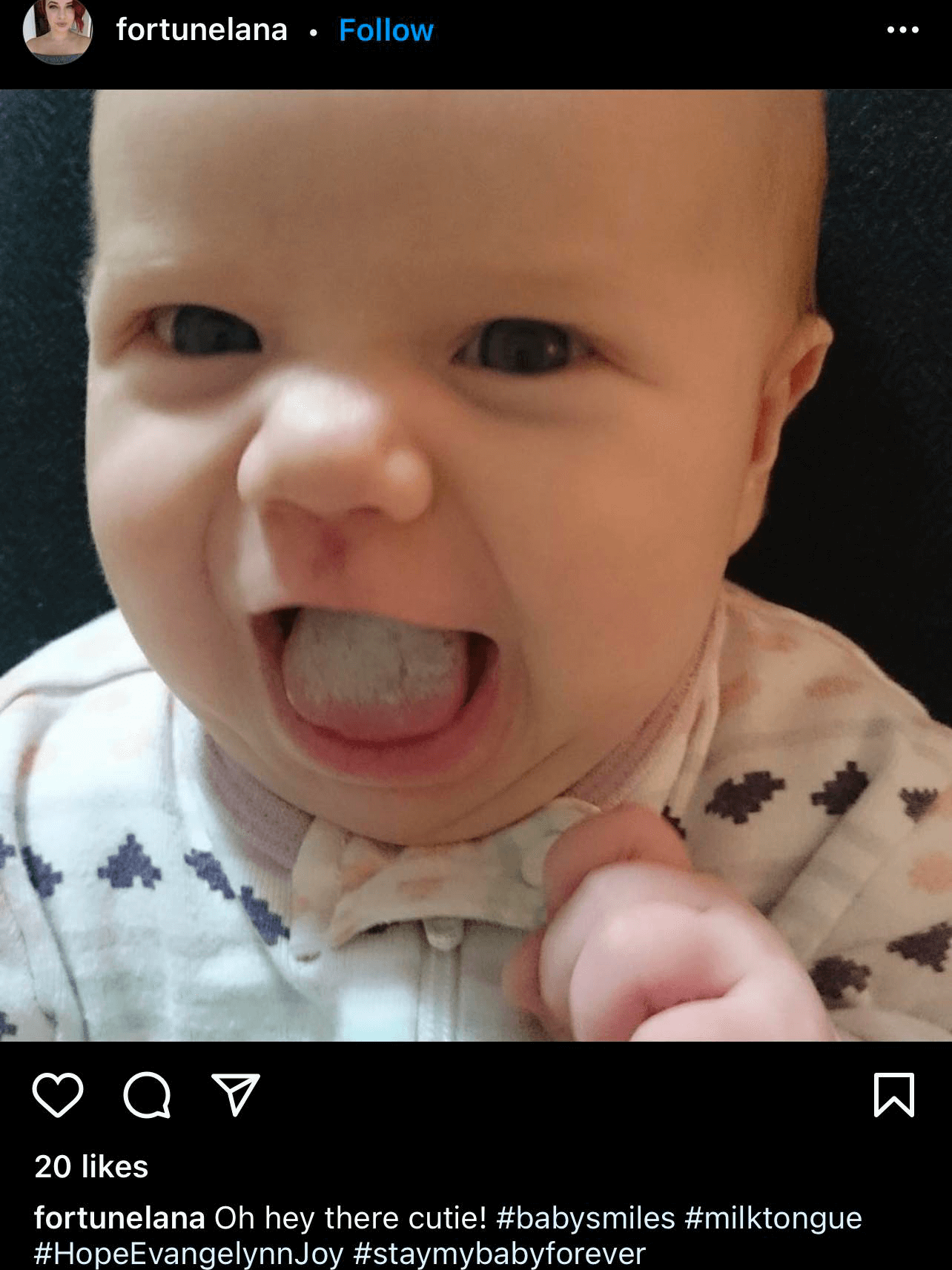
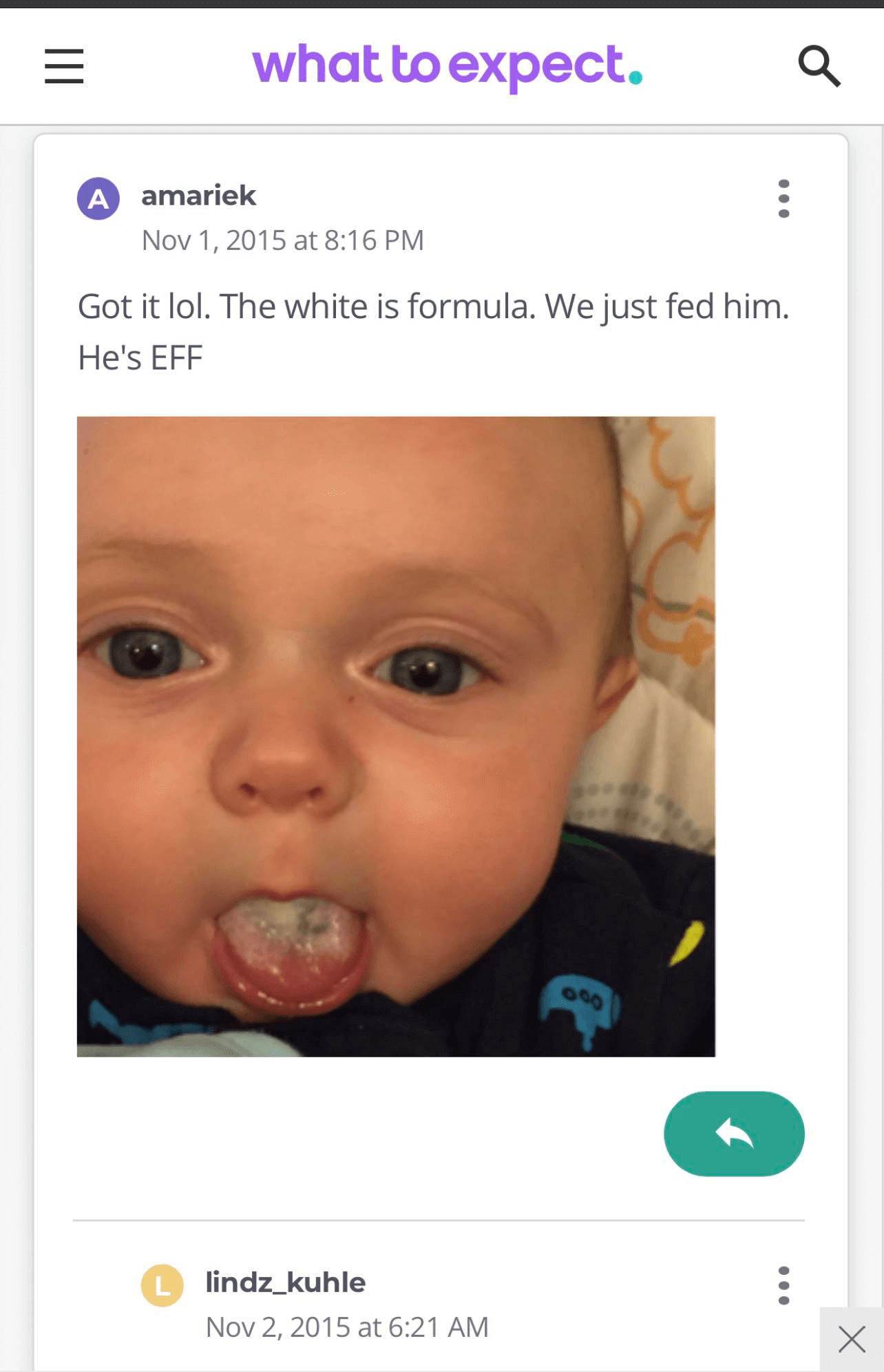
Many parents and providers confuse milk tongue with thrush. This confusion is understandable as both lead to a white coating in the mouth.
However, providers may treat both babies and parents with medications they don't need, and the primary symptoms may persist.
Milk tongue, a not-so-cute description of a tongue coated in milk residue, is due to the tongue's inability to reach the roof of the mouth, which would typically scrape off the milk film.
Milk tongue is common in babies who are tongue-tied as the tight frenulum physically prevents proper elevation.
If your baby has only a white tongue, ESPECIALLY if the tip and the sides of their tongue are nice and pink without any whiteness or signs of irritation, odds are high that thrush is NOT the issue.
Thrush vs. Black hairy tongue
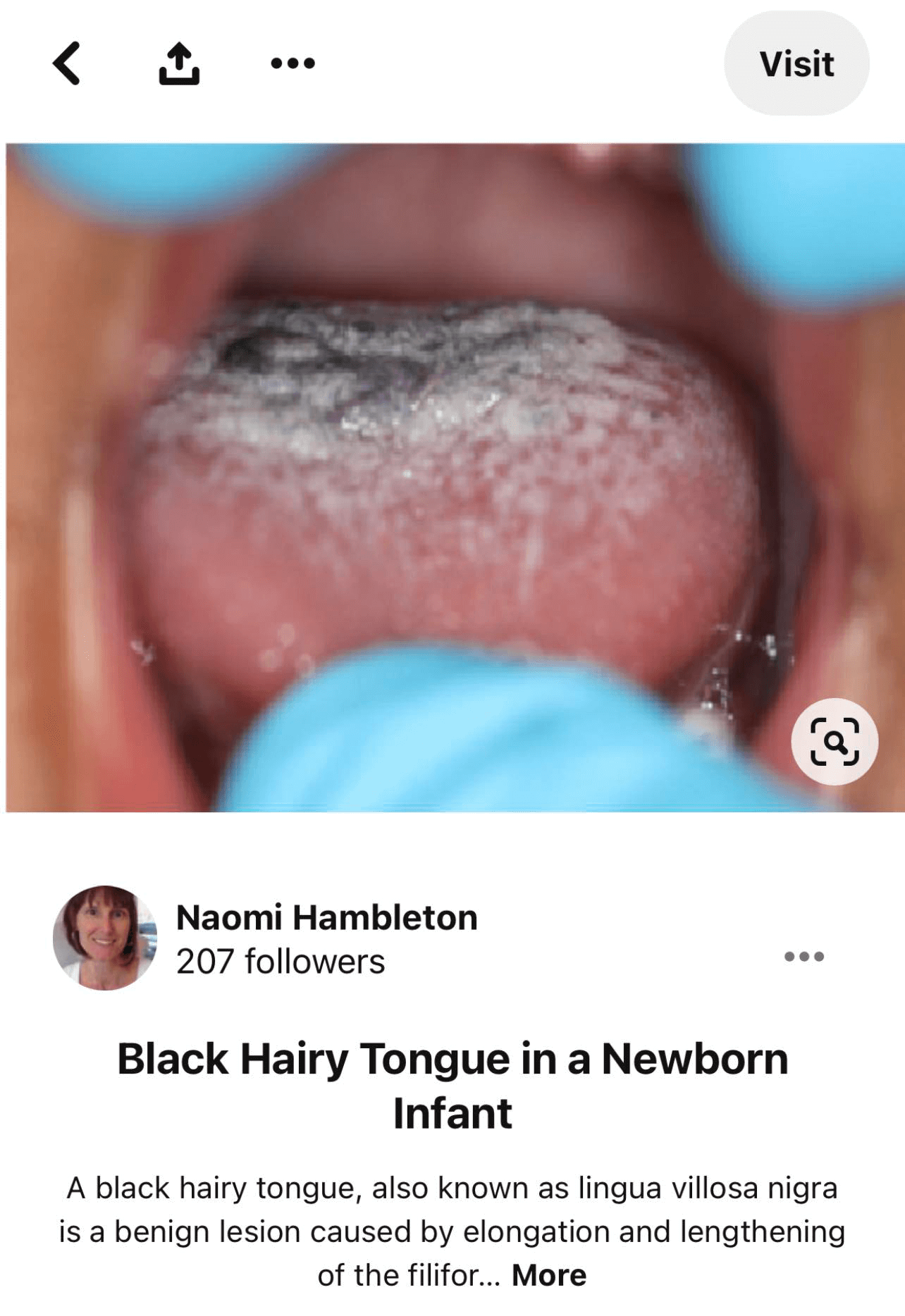
Sometimes the tongue may have a white & black coating on the surface, which may or may not look furry. If that is what prompted you to search for thrush information, congratulations, thrush is not an issue for your babe!
Instead, their milk tongue may have leveled up to black hairy tongue, an accurate, albeit disgusting description, for a tongue covered in a bacteria/ yeast biofilm.
Merely brushing your baby's tongue daily with a soft-bristled toothbrush or cloth will remove the film.
For both milk tongue and black hairy tongue, reaching out to a lactation consultant would be beneficial as they can help address the lack of tongue lift (mobility), which may cause some of the symptoms you're seeing.
Symptoms in the Breast/Chest
Controversial statement incoming...
If you're experiencing breast pain but your baby does NOT have any cottony, curdy patches in their mouth, you probably don't have thrush ( mammary candidiasis/ intraductal yeast).
Even if you any or all of the following symptoms:
Redness or itching of the nipple or areola
Deep or shooting breast pain during or between feedings
Burning pain during, after, or between feedings
Excessive dryness, shininess, or bumps on the areola
It's even more likely NOT to be thrush if you've already been treated with an antifungal and the above symptoms return, even if they subsided for a bit.
Confusing statement incoming...
If your baby does have white patches in their mouth consistent with thrush, the breast pain you're experiencing may not be thrush.
In the past few years, compelling research has come out debating the idea that many of the typical symptoms associated with thrush are due to an overgrowth of Candida. Some studies refute the idea that Candida can become pathogenic in the ducts of the mammary gland.
The challenge with identifying yeast as the cause of breast pain is that, as mentioned above, many of us naturally have Candida Albicans and the other yeast species living on our skin. The presence of the yeast is not an indication of an overgrowth of it.
A study conducted in 2016 attempted to test whether using a molecule-based test was more effective than traditional milk cultures for identifying a candida infection. In parents who showed no signs or symptoms of a thrush infection, 9.3% had positive cultures; Of the same group, 79.1% were positive using their new technique.
More confusingly, in the same study, which attempted to identify Candida overgrowth in a group of parents with breast symptoms typical of thrush, Cultures only provided evidence of a fungal infection in 8.8% of parents.
So of those who complained of thrush symptoms, both culture (8.8%) and the study's new technique (67.4%) of identification showed fewer positives than the control (non-symptom) group.
What causes the deep burning breast pain then if it's not thrush?
Based on the study and others, it's likely that the offender may be mammary dysbiosis- a fancy way of saying that the ecosystem in the breast may become disrupted, causing bacteria to wreak havoc.
So instead of yeast, you can blame bacteria, specifically Staph. Though it didn't account for all of the cases, roughly 20% of those with symptoms were positive for S. epidermidis & S. aureus. So whereas 19 of those with symptoms had either the staph strains mentioned above, only four without signs did.
"But if my baby has thrush, how would my breast pain NOT be caused by thrush" you may be asking.
If you are, you're definitely not alone.
One of the exciting but maybe not so fun things about the breast microbiome is that there may be cross-species communication.
Yeast, such as Candida Albicans, introduced to your breast/chest via contact with your baby's mouth when breastfeeding, can talk to Staph and encourage them to build a biofilm, leading to a disruption of the ecosystem. Viola! Mammary Dysbiosis, aka subacute mastitis!
Thrush vs. Mastitis
While subacute mastitis might be confused for thrush, the symptoms of traditional mastitis differ significantly from thrush.
I've written on mastitis at length previously, but in short, mastitis usually only affects one breast and will result in redness/red streaking, heat pain, swelling, and at times, a fever. Thrush generally doesn't lead to systemic symptoms such as fever.
It more commonly affects both breasts; assuming the classic symptoms are, in fact, due to thrush, it will lead to deep burning pain and redness/shininess of just the nipple/areola.
Treatment
There are many treatment options available for thrush, all with varying effectiveness & accessibility. To make things as easy as possible for you as a reader, I've broken treatment options for both parents & babies into three main categories: Prescription, Over-the-counter, and Off-label.
Please note that I am not suggesting any one particular treatment option, only providing information on the more common remedies you might see discussed in parenting groups or recommended by your care provider.
For lactation-specific guidance, I have referred to Thomas Hales' Medication & Mother's Milk.
Parents:
Prescription
Fluconazole (Diflucan): Fluconazole may be prescribed as an oral suspension or a tablet and is used to treat both oral, vaginal, or nipple yeast. The way Fluconazole works in treating yeast is well known- it blocks the yeast's ability to reproduce.
While Fluconazole effectively treats thrush, especially compared to nystatin creams, it can be expensive and has more risk of side effects than topical creams.
Even for high doses of Fluconazole, the amount of the medication passed through the milk is less than the usual pediatric dosage of Fluconazole. Consequently, Hale rates this medication as safe (L2), but all parents should be aware that GI upset is possible for both the person taking it and an infant receiving their milk.
Nystatin: While all Nystatin is via prescription only, Nystatin cream to treat nipple thrush differs from the Nystatin suspension used to treat infant oral thrush. As with all prescription medications, it's essential to use Nystatin for as long as guided by your provider.
You do not need to wipe Nystatin off before feeding, and hale lists it as L1 (safest). Despite arguments against its efficacy compared to other treatment options, it's the most common first-line treatment for nipple thrush in the US due to its safety and low cost.
Over the counter
Miconazole: Topical Miconazole cream is a popular first-line choice for nipple thrush in the UK. Miconazole cream is often the active ingredient in OTC fungal creams such as Monistat 7, a vaginal yeast cream in the US. In some cases, Miconazole is available only by prescription.
General advice with Miconzole is to apply right after feeding and have a breast pad barrier between nipple and bra/shirt. In most cases, there is no need to wipe off the nipple before the next feed, but if you note excess cream on your nipple, it may be worth gently wiping off.
Some sources recommend against Miconazole usage while human milk feeding. However, topical application to the nipples or even intravaginal use- a method that leads to more absorption- is unlikely to lead to notable medication levels in milk. And because once ingested, oral absorption by the baby is low, Hale has Miconazole classified as L2.
Probiotics: The evidence to support probiotic usage for C. albicans infections are growing, chiefly focusing on finding which probiotic is best for each specific situation.
There are many probiotic strains & it's beyond this post's scope to look at each Probiotic family. However, two note-worthy genera are Lactobacillus and Bifidobacterium, which can be easily found in over-the-counter probiotic blends and foods sold at the average grocery store.
And as we wait for stand-alone studies that show probiotics as a viable solution to nipple yeast independent of other treatment, the current research shows quicker resolution of yeast when probiotics are used in conjunction with Fluconazole.
Coconut oil: Coconut oil is an effective antifungal and may be effective against C. albicans. Considering most parents have coconut oil at home, this may be an excellent first-line "natural" option. Whether or not it works well when applied to the nipples remains unproven via science, but some parents swear by it.
You will not need to wipe off before nursing or pumping.
Off Label
Monistat 7 & Micatin are two topical yeast creams with specific uses that are not specific to nipple/breast yeast. The active ingredient is Miconazole (see above).
Lotrimin AF: Lotrimin AF is one brand name of Clotrimazole, a topical antifungal cream used to treat Athlete's foot. Other variations of Lotrimin are available and used to remedy vaginal yeast, jock itch, and diaper rash.
If using Lotrimin to treat nipple thrush, wash off before nursing or pumping.
Infant
Prescription
Nystatin oral suspension: Nystatin oral suspension is the mode of administration used for infants. Your provider will guide you on specific dosing, though generally, the application will be multiple times a day.
GI upset, diarrhea, and vomiting are possible side effects.
Diflucan oral Suspension: Another mode of administration of Fluconazole, providers may suggest this rather than Nystatin in places like the UK.
For severe cases of yeast and/or for older babies, Ketoconazole or itraconazole may be prescribed.
Over the counter
Gentian Violet: Gentian Violet Dye is an evidence-based approach many parents use to treat oral thrush, and with it being over the counter, purple-stained baby mouths are not uncommon to see.
Because there are different concentrations of Gentian Violet, it's essential to ensure that the GV you've got is no more than 1%. Higher concentrations come with increased risks of creating ulcers in your baby's mouth.
A small study showed that concentrations as low as 0.00165% were effective in treating thrush and with the added benefit of no oral staining; however, researchers conducted this study on adults & not babies.
Miconazole Gel (Daktarin): Like Miconazole cream, UK providers may prefer Miconazole Gel over Nystatin Suspension to treat oral Candida in infants. As US pharmacies don't sell Miconazole Gel, it may be harder to get than Gentian Violet for parents in the US.
Do you and your baby both need to be treated at the same time?
Questions about simultaneous treatment are not uncommon, and up until recently, my answer would have always been yes; if you suspect thrush, treat baby even if no white plaques are present in your baby's mouth.
The reverse held as well; if your baby has oral thrush, treat everything that comes into contact with their mouth, including your nipples.
As more information has come to light about the causes of breast & nipple pain and the possibility thrush is not even the most likely cause, I think it's worth considering that in some cases, topical nipple treatment may be all that's necessary.
Because oral thrush can disrupt bacteria count, nipple pain secondary to oral thrush is probably worth treating simultaneously.
It's up to each parent to weigh the benefits/ risks of treatment in the absence of symptoms.
If your baby has oral plaques consistent with oral thrush, sanitizing everything that comes into contact with their mouth after usage can speed up the treatment process.
If you have a vaginal yeast infection and your baby has pronounced thrush, dual treatment would be warranted. Ensure to pay attention that no other people- such as sexual partners- have the opportunity to prolong the infection.
Example: Oral sex during yeast infection then sometime later, "cleaning" a paci by sucking on it.
What if you do nothing?
For oral thrush in full-term healthy babies, thrush may resolve on its own without any treatment. The treatment of time may be an option for babies who don't have any pain or difficulties feeding.
The United States generally suggests the "wait-and-see" approach less frequently than other parts of the world but is an option for all minor oral thrush cases.
For breast pain that is unresolved despite latch & positioning changes, further investigation of the cause is always recommended. This extends to persistent breast pain despite thrush treatment as well.
Have you dealt with thrush? What remedy did you find the most helpful?